Medicaid is the single largest payer for mental health services in the United States, playing a critical role in ensuring access to care for millions of adults with mental illness and substance use disorders. An estimated 58.7 million U.S. adults—nearly one in four—live with a mental illness, according to national health data. Among this population, individuals enrolled in Medicaid are more likely to experience mental illness than those with private insurance, underscoring the program’s central role in combatting America’s mental health crisis.
While Medicaid is federally funded, it is administered by individual states, each of which has broad discretion over how it structures, finances, and delivers services. As a result, the availability and quality of behavioral health services can vary significantly from state to state. These differences are especially important now, as many states face financial pressures and potential budget cuts that could make it harder for people to access the care they need.
This analysis by Addiction-Rep—a consulting firm specializing in the behavioral health sector—draws on data from the Substance Abuse and Mental Health Services Administration (SAMHSA), Centers for Disease Control and Prevention (CDC), and Centers for Medicare and Medicaid Services (CMS). It examines how the prevalence of mental illness has changed over time, highlights its disproportionate impact on low-income individuals and Medicaid enrollees, and ranks state Medicaid programs based on their performance across key behavioral health indicators.
The Prevalence of Mental Illness in the U.S.
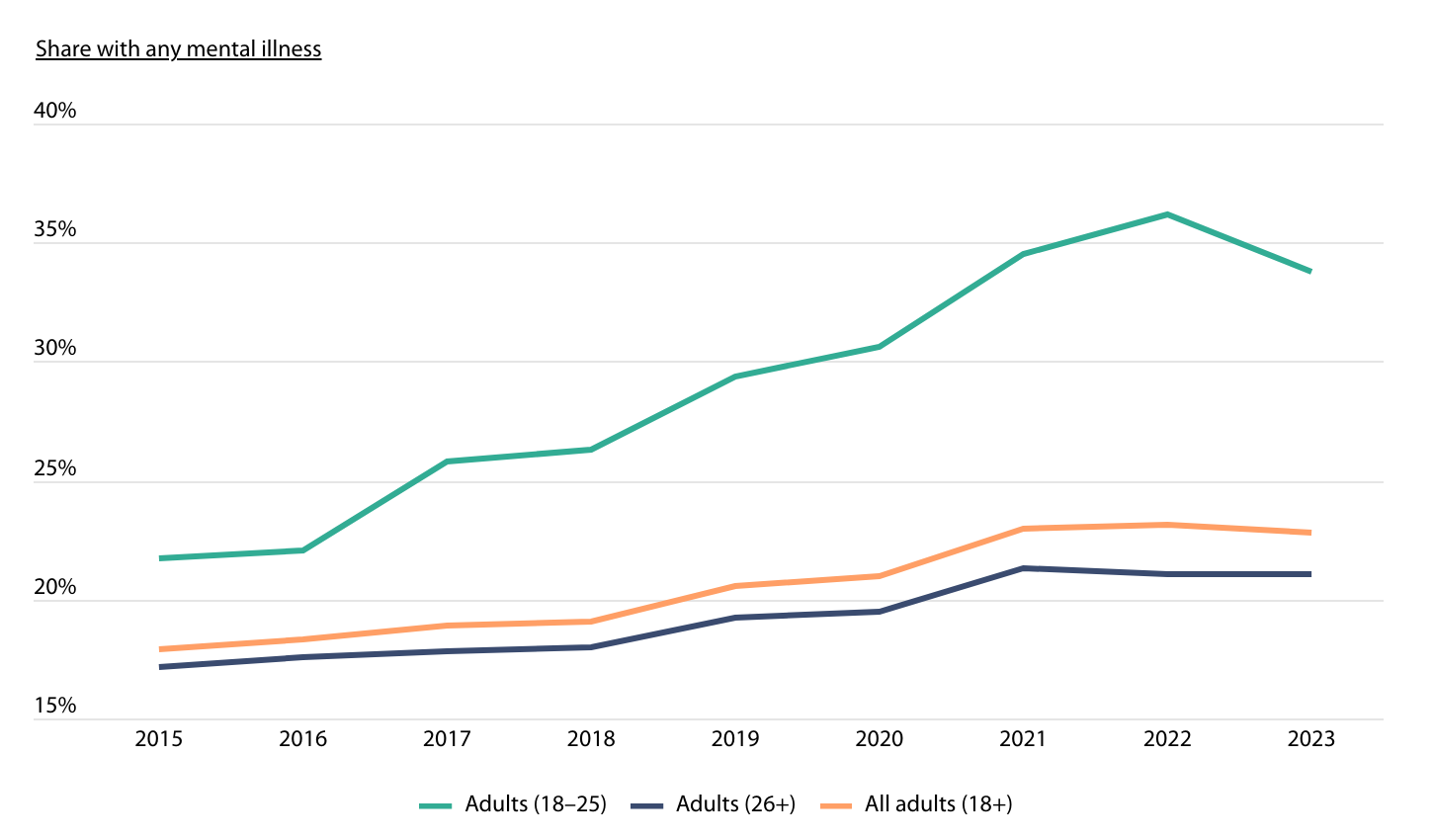
Source: Addiction-Rep analysis of Substance Abuse and Mental Health Services Administration data | Image Credit: Addiction-Rep
The United States is facing a sustained mental health crisis, marked by a steady rise in the share of adults experiencing mental illness over the past decade. In 2015, about 17.9% of adults reported a mental illness, according to data from SAMHSA. By 2023, that figure had climbed by more than a quarter to 22.8%.
Young adults between the ages of 18 and 25 have been disproportionately impacted. Their rate of mental illness rose from 21.7% in 2015 to a peak of 36.2% in 2022, before dipping slightly to 33.8% in 2023. Meanwhile, adults aged 26 and older saw more gradual increases, rising from 17.2% in 2015 to 21.1% in 2023.
Outside of age, income is also an important factor impacting the prevalence of mental illness. National health data from the CDC shows that in 2023, nearly one in five adults living below the federal poverty line (19.4%) reported regularly feeling worried, nervous, or anxious. That compares to 15.8% of those with incomes between 100% and 199% of the poverty line, and just 10.7% of adults with incomes at or above 200% of the poverty line.
The Importance of Medicaid in Treating Mental Illness
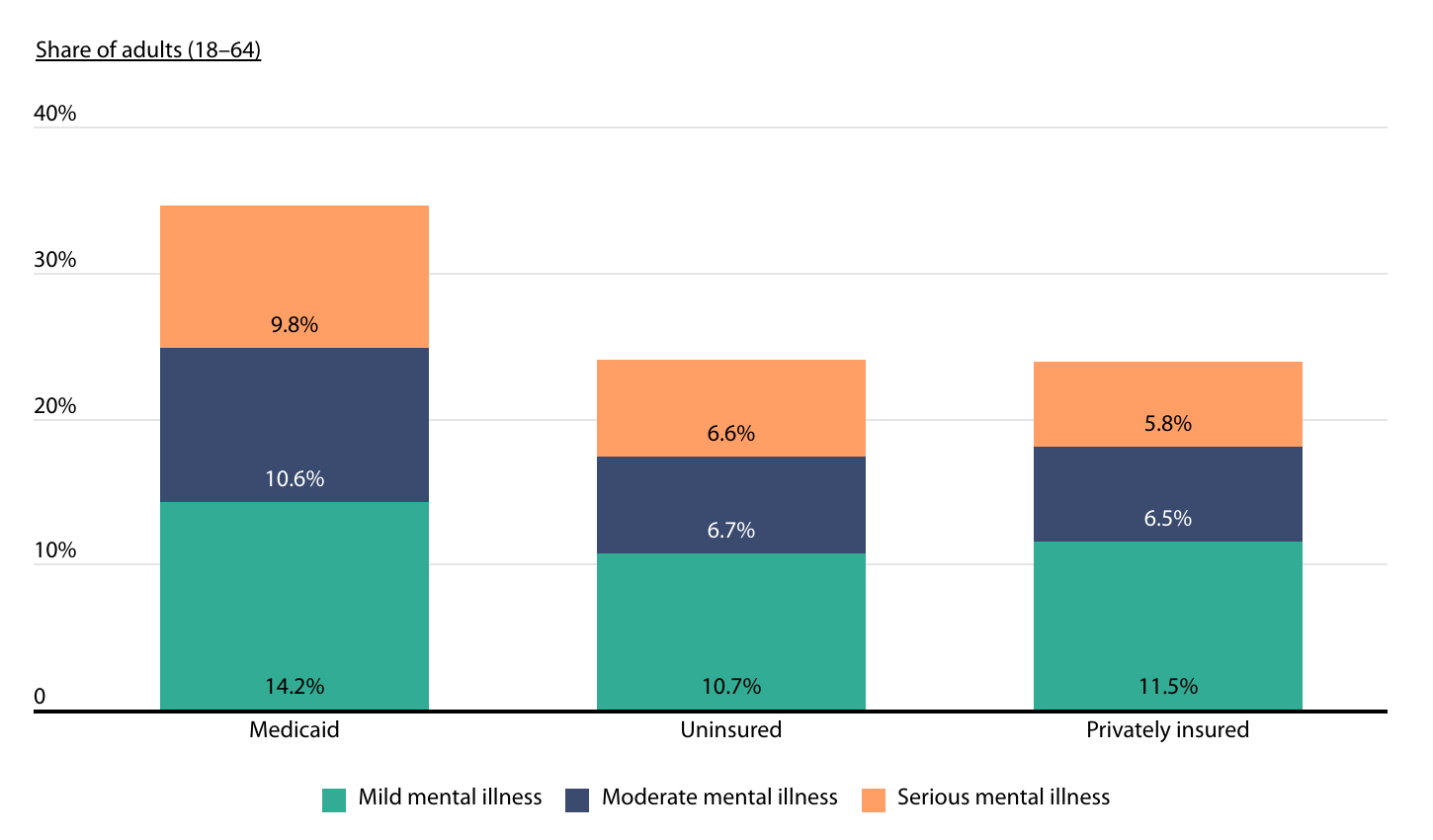
Source: Addiction-Rep analysis of Substance Abuse and Mental Health Services Administration data | Image Credit: Addiction-Rep
As a result of these differences, Medicaid plays an outsized role in connecting Americans with mental illness to care. In 2023, 34.6% of adults enrolled in Medicaid experienced some form of mental illness, compared to 24.0% of uninsured adults and about 23.9% of those with private insurance, according to SAMHSA data.
The gap is even more pronounced when looking specifically at serious mental illnesses, such as bipolar disorder, major depressive disorder, and schizophrenia. Nearly one in 10 Medicaid enrollees (9.8%) reported having a serious mental illness in 2023, compared to 6.6% of uninsured adults and just 5.8% of adults with private insurance.
State Medicaid Programs With the Best Mental Health Care
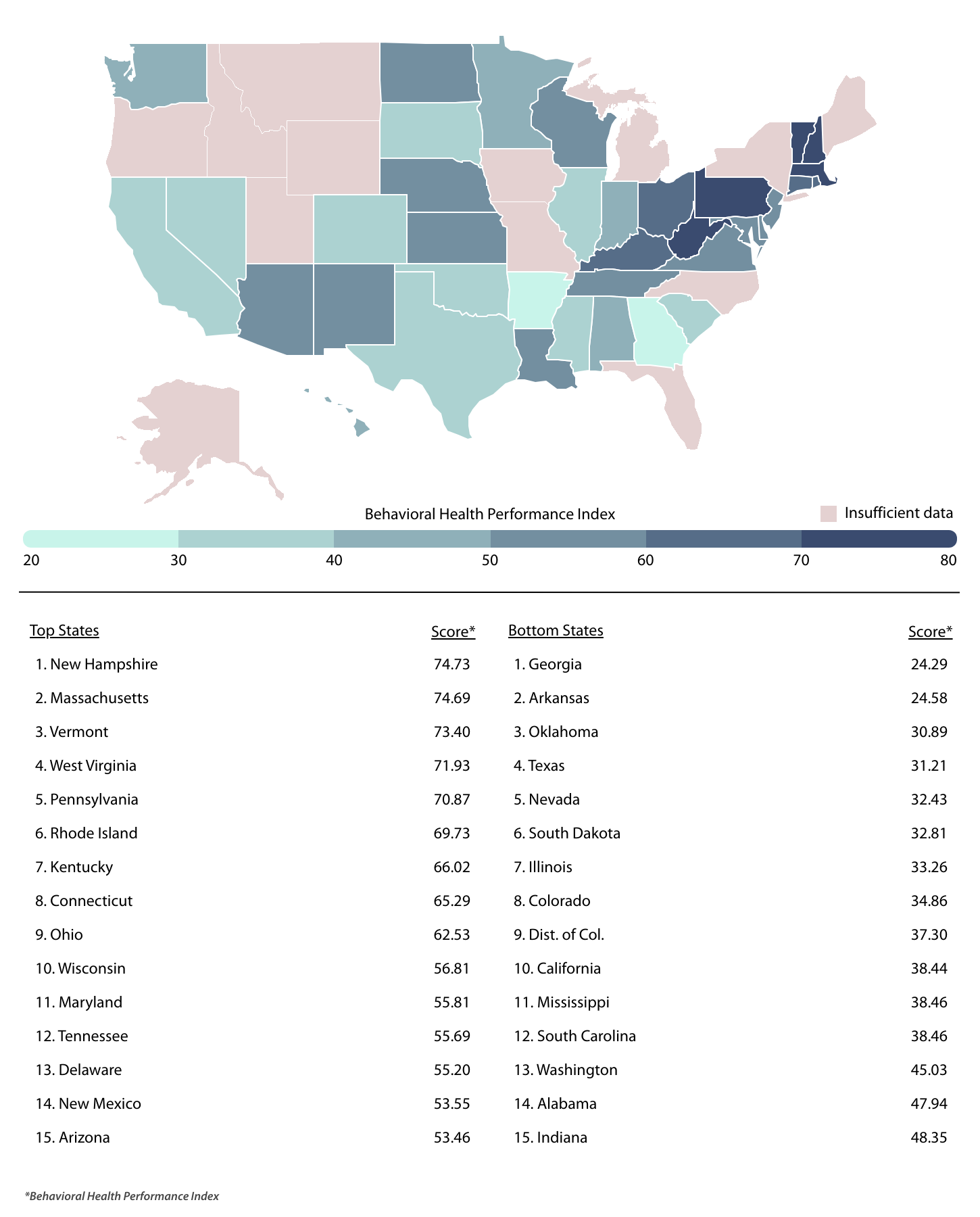
Source: Addiction-Rep analysis of CMS data | Image Credit: Addiction-Rep
To assess how state Medicaid programs perform in delivering behavioral health care, researchers at Addiction-Rep developed a composite score—the Behavioral Health Performance Index. This index ranks states based on a range of quality measures grouped into four categories: initiation and engagement, evidence-based medication use, care continuity and follow-up, and patient experience.
The specific metrics within each category are detailed in the methodology section below, but they include key indicators such as how often patients receive timely follow-up care after emergency department visits for mental illness, the rates at which individuals initiate and stay engaged in substance use disorder treatment, and the use of FDA-approved medications—like buprenorphine or methadone—for treating opioid use disorder, among others.
The top-performing states are heavily concentrated in the Northeast and parts of Appalachia. New Hampshire, Massachusetts, and Vermont rank first, second, and third respectively, each earning a Behavioral Health Performance Index score above 73. These states consistently performed well on metrics related to initiation, follow-up care, and evidence-based medication use, but scored lower on patient experience. West Virginia and Pennsylvania round out the top five, demonstrating stronger performance with regard to patient experience, but scoring slightly lower in other categories.
By contrast, several large and populous states landed near the bottom of the rankings. California, Texas, Illinois, and Georgia all appeared in the bottom 10, along with states like Arkansas and Oklahoma. California stood out for its strong performance in the use of evidence-based medications and follow-up care after behavioral health episodes, but it scored poorly on treatment initiation and patient experience—pulling down its overall ranking. Other lower-performing states tended to show more consistently weak results.
For complete results across all states with available data, see the original post on Addiction-Rep: Ranking State Medicaid Programs on Mental Health: Where Does Your State Stand?
Methodology

Photo Credit: Andrei R / Shutterstock
This analysis evaluates how effectively state Medicaid programs serve adult patients with mental health and substance use needs, based on data from the Centers for Medicare and Medicaid Services (CMS) Medicaid and CHIP Scorecard – Core Set Year 2023. To compare performance across states, Addiction-Rep developed a composite score called the Behavioral Health Performance Index. This index averages scores across four key categories: initiation and engagement, evidence-based medication use, care continuity and follow-up, and patient experience.
Each category consists of multiple metrics, most of which focus on adult behavioral health patients aged 18 to 64. However, patient experience measures apply to all adult Medicaid enrollees, as condition-specific experience data is not available. Only states with sufficient data across all four categories were included in the final rankings. However, states with partial data are still shown in visualizations and detailed tables for the metrics where data is available.
Below is a breakdown of the metrics included in the final index, organized by category, along with descriptions of each:
Initiation & Engagement
- SUD Initiation (14d): Share of new substance use disorder (SUD) treatment episodes where the patient began treatment within 14 days of diagnosis.
- SUD Engagement (34d): Share of new SUD treatment episodes where the patient attended additional treatment within 34 days of starting care.
Evidence-Based Medication Use
- OUD Pharmacotherapy: Share of adults with opioid use disorder (OUD) who received FDA-approved medication-based treatment options, such as buprenorphine or methadone.
- Antidepressant Acute Adherence (12w): Share of adults with major depression who remained on prescribed antidepressants during the initial 12-week treatment phase.
- Antidepressant Continuation Adherence (6m): Share of adults with major depression who remained on prescribed antidepressants through a six-month treatment period.
- Antipsychotic Adherence: Share of adults with schizophrenia or schizoaffective disorder who remained on prescribed antipsychotic medications for at least 80% of their treatment duration.
Care Continuity & Follow-Up
- SUD/Overdose ED Follow-Up (7d): Share of emergency department visits for substance use or drug overdose with a follow-up visit within seven days.
- Mental Health ED Follow-Up (7d): Share of emergency visits for mental illness or intentional self-harm with a follow-up visit within seven days.
- Mental Health Hospital Follow-Up (7d): Share of adults discharged after hospitalization for mental illness or self-harm who had a follow-up visit within seven days.
Patient Experience
- Health Care Satisfaction (9–10 Rating): Share of adults who rated their overall health care experience as a 9 or 10 on a 10-point scale.
- Health Plan Satisfaction (9–10 Rating): Share of adults who rated their Medicaid health plan as a 9 or 10 out of 10.
- Always Got Needed Care: Share of adults who reported “always” getting the care they needed, based on a four-point response scale ranging from “never” to “always.”
For complete results, see Ranking State Medicaid Programs on Mental Health: Where Does Your State Stand? on Addiction-Rep.





